Gene therapy: New strategy against hereditary blindness
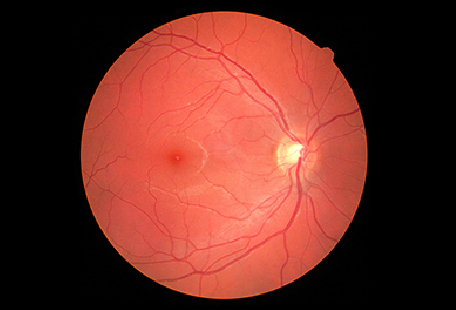 Retinitis pigmentosa leads to the death of the light-sensitive cells of the retina. Photo: Jevgenij / AdobeStock
Retinitis pigmentosa leads to the death of the light-sensitive cells of the retina. Photo: Jevgenij / AdobeStock
In Germany, up to 40,000 people are affected by the hereditary eye disease retinitis pigmentosa, which is caused by mutations in numerous different genes. Depending on the genetic defect, there is night blindness and a gradual loss of field of vision or even complete blindness. The first gene therapeutics were recently approved for certain forms of the disease. However, conventional gene therapies have disadvantages that limit their possible uses. For this reason, a team led by private lecturer Elvir Becirovic at the Chair of Pharmacology of Natural Sciences (headed by Prof. Dr. Martin Biel) has developed a new strategy in which they use CRISPR / Cas9 technology to reactivate decommissioned genes that have similar functions to the defective genes fulfill. Also involved in the development was Prof. Dr. Stylianos Michalakis from the Eye Clinic of the LMU Munich. They successfully tested their new gene therapy approach in a mouse model, as the scientists report in the journal Science Advances.
Two strategies are currently used in the development of gene therapies: As part of gene supplementation, attempts are made to replace the defective gene with an intact version. However, this is currently only possible for relatively small genes. The second strategy aims to correct mutations that cause disease, but this usually has to be tailored for each individual mutation. In view of the high level of effort and the associated development costs, broad use of this strategy is therefore not possible. "To overcome these limitations, we have developed a completely new strategy," says Becirovic.
Many genes in the human genome have similar functions, but they are often active at different times or in different cells. "Our idea was to compensate for the function of a mutant gene by using the so-called Cas9-VPR system to switch on genes that were actually shut down with a similar function in the affected cells," says Becirovic. The Cas-9-VPR system is a variant of the well-known CRISPR / Cas9 technology, with it the genome can be changed without cutting it up.
The scientists successfully used this new method in a mouse model for retinitis pigmentosa: The mice carry a mutation in a gene for the visual pigment rhodopsin. This pigment is produced exclusively in the rods, i.e. in the visual cells that are responsible for night and twilight vision. By injecting Cas9-VPR into the rods of the mice, the scientists switched on genes closely related to the rhodopsin gene, which are normally active in the cones responsible for color and daytime vision. “This enabled us to compensate for the lack of rhodopsin function, slow down the degenerative process of retinitis pigmentosa and improve retinal function without any detectable side effects,” says Becirovic.
According to the scientists, the new approach can also be applied to numerous other genes and hereditary diseases and offers decisive advantages compared to the existing strategies. "In view of the rapidly growing importance of gene therapy and the associated benefits for those affected, we are convinced that our approach could soon be used in the first clinical feasibility studies," says Becirovic.
Science Advances 2020